follow-up case reports
In research applications brain4care offered a critical vital sign to a patient's clinical context in real time for an unlimited amount of time, in a non-invasive way, with no pain and non significant risks
vps valve adjustment
Application and context
Hydrocephalus is a disease caused by abnormal accumulation of cerebrospinal fluid in the brain in one or more ventricular sinuses, causing a change in brain compliance. The clinical follow-up of this disease includes periodic evaluation of surgically implanted valve function in patients to regulate adequate CSF drainage and maintain central nervous system balance (VPS valve).
Without a simple non-invasive technology, valve adjustment is done by observing the clinical condition in a trial-and-error basis until adequate flow is achieved. This process requires recurring patient office visits that may take from weeks to months.
how brain4care may contributes to the adjustment or replacement of vps valves
- When the patient’s symptoms worsen when they are lying down, and the ICP surrogate waveform is altered in this position, this may be a sign that the valve is not providing the necessary flow
- If the symptoms worsen when the patient is seated and the surrogate ICP waveform changes in this position, this is a sign that the valve may be draining more than necessary
- Monitoring can be performed in minutes, in various care settings, without causing pain or entailing risks to the patient
- Allows the reduction of the time to reach the valve’s adequate flow from months to hours or days
- Drastically reduces the need for patient and caregiver transport
- Optimizes the office’s agenda by opening space to work on new cases
- More safety and assertiveness in the surgical indication for shunt replacement
clinical case 1 – vps valve control
Patient with ventriculoperitoneal shunt (VPS) complaining of severe headaches.
The noninvasive intracranial pressure monitoring (NIICP) was requested by clinician for evaluation of the VPS and respective follow-up with a diagnostic hypothesis of alteration of the VPS drainage flow.
findings and medical procedure
first monitoring
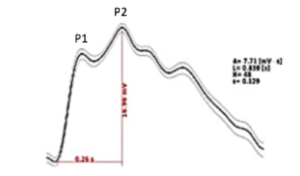
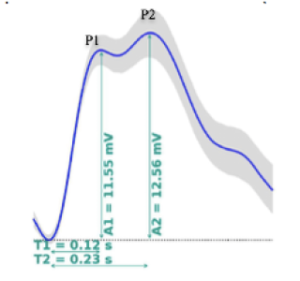
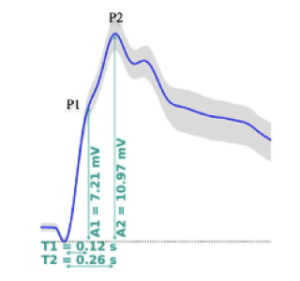
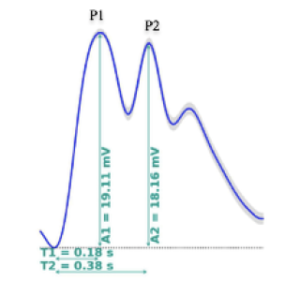
Change in surrogate ICP waveform (P2/P1 ratio > 0.8)
medical procedure
Adjustment of the CSF drain valve in the VPS to 10 cmH20
second monitoring
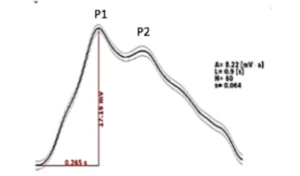
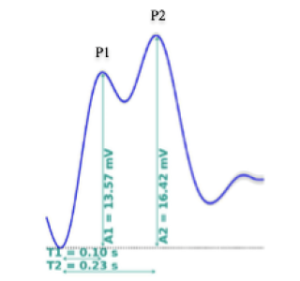
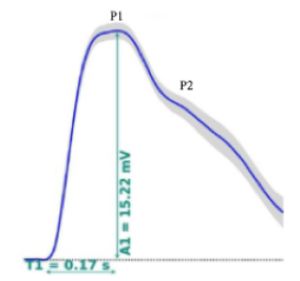
Surrogate ICP waveform within normal parameters (P2/P1 ratio < 0.8)
medical procedure
Maintain the CSF drain valve in the VPS at 10 cmH20
outcome
Improvement of patient quality of life. Elimination of pain and constant visits to emergency rooms.
clinical case 2 – vps valve gauging
Young female with a history of hydrocephalus. Ventriculoperitoneal drainage valve procedure performed approximately 1 year ago. Subject maintained a stable clinical situation during the entire period after the VPS procedure. She informed her doctor that she would be traveling and asked to undergo non-invasive intracranial pressure monitoring (NIICP) to check the proper functioning of the valve.
findings and medical procedure
first monitoring
Surrogate ICP waveform without changes (P2/P1 ratio < 0.8)

medical procedure
Patient cleared for travel.
outcome
Fast result without impacting the patient’s life, without exposure to the radiation of imaging tests and with reduced costs.
surgical procedures with extracorporeal circulation (ecc)
Application and context
During surgeries, with the use of extracorporeal circulation, there is an interruption of cerebral blood flow for an average period of 6 to 7 minutes, which increases the risks of neurological sequelae, as this alters brain compliance. For the prevention of this type of sequelae, intensive care physicians make use of several measures in the postoperative period, known by the term neuroprotection.
How brain4care contributes to the reduction of postoperative neurological sequelae
brain4care’s non-invasive monitoring method may assist the intensive care physician in monitoring postoperative ICU patients supporting he decision whether neuroprotection measures such as sedation and vasoactive drugs are playing the therapeutic role of normalizing brain compliance. This way, it may be possible to define the best moment for patient extubation, potentially reducing the risks of reversible neurological sequelae such as mild confusion and temporary loss of movement, and irreversible sequelae, such as paresis (reduction or absence of the ability to move a part or side of the body) and severe neurological sequelae (causing total or partial physical dependence on others).
potential benefits and impacts
- Ease of use of the non-invasive method by the bedside
- The morphology of the intracranial pressure curve may be used as an aid to interpretation of alteration in brain compliance and detection of intracranial hypertension.
- From monitoring to reporting in minutes
related scientific article
Determinants of neurological complications in the use of extracorporeal circulation (ECC).
Natia de Freitas Barbosa; Danilo Martins Cardinelli; Flávia Falci Ercole
Federal University of Minas Gerais, Belo Horizonte, MG – Brazil
Clinical case 1- surgical procedures with extracorporeal circulation (ecc)
Man, age 50, with a two year old aortic aneurysm procedure. Admitted for dissection of the aorta, with a surgical proposal for its correction. During the procedure, the patient underwent extracorporeal circulation for 82 minutes, with aortic clamping at 48 minutes of surgery and cerebral hypoflow for 6 minutes.
Surgical procedure occurred without any incident and, at the end, the patient was referred to the ICU, sedated, in mechanical ventilation with the use of vasoactive drugs.
Noninvasive intracranial pressure monitoring (NIICP) was requested to analyze the behavior of the intracranial pressure curve (ICP) morphology after a procedure that caused cerebral hypoperfusion and to confirm whether the neuroprotection measures were effective. The patient was monitored three times (in the immediate postoperative, first postoperative and second postoperative periods).
findings and medical conduct
first monitoring
Change in surrogate ICP waveform (P2/P1 ratio = 1.08)
medical procedure
Maintain sedation and wait 24 hours for further monitoring.
second monitoring
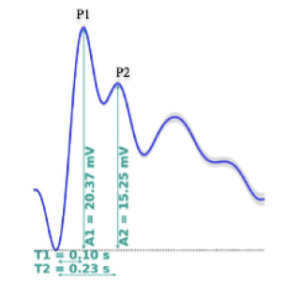
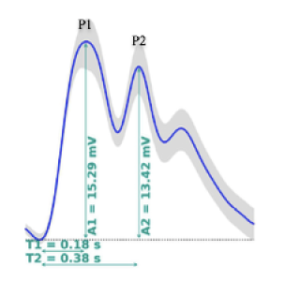
Surrogate ICP waveform change, P2> P1, with worsening in the P1/P2 ratio = 1.52
medical procedure
Optimization of the sedation scheme for neuroprotection
third monitoring
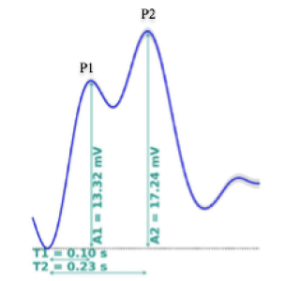
Surrogate ICP waveform within an interpreted normal range with P1> P2 (P2/P1 ratio = 0.75)
medical procedure
Sedation withdrawal and patient extubation.
outcome
Extubation of the patient in the postoperative room, without neurological sequelae and with reduced length of stay in the ICU
Clinical case 2- surgical procedures with extracorporeal circulation (ecc)
A 40-year-old man, diagnosed with Marfan’s Syndrome, with 9 yo correction of aortic dissection , was admitted with a diagnosis of tube endocarditis. The patient underwent the exchange of a valved tube plus coronary artery reimplants.
During the surgical procedure, extracorporeal circulation was done for 182 minutes, with aortic clamping at 112 minutes and cerebral hypoflow for 9 minutes.
After the procedure, he was referred to the ICU, intubated, in mechanical ventilation with vasoactive drugs. On the same day, he had a convulsive tonic-clonic seizure.
Non-invasive intracranial pressure monitoring (NIICP) was requested to monitor the effectiveness of neuroprotection measures. Overall, the patient was monitored four times (immediate postoperative, 1st postoperative, 2st postoperative, and 3rd postoperative periods).
findings and medical procedure
first monitoring
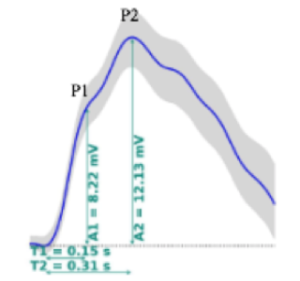
Change in surrogate ICP waveform with P2> P1 (P2/P1 ratio = 1.3)
medical procedure
Optimization of the sedation scheme and prevention of secondary cerebral ischemia.
second monitoring
Performed in the first postoperative period. Maintained surrogate ICP waveform with P2> P1, but with an improvement in the P2/P1 ratio (P2/P1 ratio = 1.21).
medical procedure
Optimization of the sedation scheme for neuroprotection.
third monitoring
Performed in the second postoperative period. Progression of the condition with improvement of surrogate ICP waveform, however, P2>P1 (P2/P1 ratio = 0.95).
medical procedure
Maintain sedation and monitor again in 48 hours.
fourth monitoring
Performed in the postoperative period. Patient responded well to neuroprotection and the morphology of surrogate ICP waveform is almost normalized, P2/P1 = 0.87.
medical procedure
Remove sedation and wait for extubation.
outcome
Patient was extubated on the fifth day of inpatient care and did not present neurological deficits.
neuroprotection after cardiac arrest
Application and context
After cardiac arrest, there is an interruption of brain blood flow and, consequently, a change in cerebral compliance. The death rate of patients in this state can reach up to 80% and it is known that 8 out of 10 survivors will have neurological sequelae. For prevention of sequelae of this type, intensive care physicians use several post-arrest measures known by the term neuroprotection, reducing the rate of survivors with sequelae to 2 out of 10 patients.
How brain4care contributes to the prevention of post-stop neurological sequelae
brain4care’s non-invasive monitoring method may assist the intensive care physician in monitoring post-arrest ICU patients, determining whether neuroprotection measures such as sedation and vasoactive drugs are playing the therapeutic role of normalizing brain compliance. This way, it may be possible to define the best moment for extubation of the patient, reducing the risks of reversible neurological sequelae such as mild confusion and temporary loss of movement, and irreversible sequelae, such as paresis (reduction or absence of the ability to move a part or side of the body) and severe neurological sequelae (causing total or partial physical dependence on others).
main benefits and impacts
- Ease of use of the non-invasive method at bedside
- The morphology of the intracranial pressure curve may be used as a marker to detect alteration in brain compliance and to detect intracranial hypertension
- From monitoring to reporting in minutes
related scientific article
Determinants of neurological complications in the use of extracorporeal circulation (ECC).
Natia de Freitas Barbosa; Danilo Martins Cardinelli; Flávia Falci Ercole
Federal University of Minas Gerais, Belo Horizonte, MG – Brazil
Clinical case 1 – neuroprotection after cardio-respiratory arrest
Man, age 64, with diagnosis of invasive tubular adenocarcinoma barely differentiated from sigmoid. Patient underwent electrosurgery with TT anastomosis without incident, referred to the bed after the anesthesia recovery period.
On the same day, after 1 hour in the recovery ward, he presented cardiorespiratory arrest in EAWP (electrical activity without pulse), with return of heart rhythm after 8 minutes of resuscitation maneuvers according to the ACLS (Advanced Cardiac Life Support) guidelines.
The patient, hemodynamically stable, was referred to the ICU and started neuroprotection measures for 24 hours: sedation and analgesia, temperature control (between 35-36ºC), glycemic control, PCO2 (partial pressure of carbon dioxide) between 35 and 40 mmHg, continuous capnography, hydration seeking VPS (mean arterial pressure) between 8 and 12 mmHg, AAP (Average Artery Pressure) between 90 and 100 mmHg, noninvasive monitoring of continuous cardiac output, oxygen saturation above 94%, plasma sodium above 140 mEq/L, continuous electroencephalogram, monitoring of NIICP (noninvasive intracranial pressure) prior to initiation of sedation and after complete withdrawal of sedation. The monitoring of NIICP was requested to verify whether the neuroprotection measures were effective to reduce possible brain damages caused by the cardiac arrest.
findings and medical procedure
first monitoring
Change in surrogate ICP waveform (P2/P1 ratio = 1.46)
medical procedure
Initiate sedation and other neuroprotection measures according to medical prescription.
second monitoring
Surrogate ICP waveform changed (P2/P1 ratio = 0.64).
medical procedure
Initiate withdrawal of sedation for extubation.
outcome
Extubation of the patient in the postoperative room, without neurological sequelae and with reduced length of stay in the ICU.