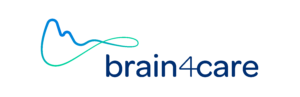
vital signs
Key health indicators
Maintaining our health is an ancestral universal need. Over time human beings have learned to access and understand signs that indicate when vital functions are altered, i.e., our vital signs.
With the latter we make decisions that keep us from getting sick or cure us from a diseases, expanding our ability to live longer and better.
When we measure our body temperature and identify a fever, we know what it means and what to do, thus making decisions to keep us healthy. The same happens with respiratory and heart rate, blood pressure and pain of known origin.
Before we had this knowledge death from trivial clinical occurrences was not uncommon. Establishing a new vital sign means providing additional and supplementary information to reestablish and maintain health, doing good for all continuously.
Access to indicators that monitor changes in key brain vital signs such as intracranial pressure (ICP) and intracranial compliance was only possible with the surgical introduction of a catheter through piercing of the skull with obvious restrictions of use.
brain4care pioneers the non-invasive access to a the surrogate ICP waveform. This waveform serves as a complementary information in clinical contexts that require monitoring of ICP over time with potential of support cases of: aneurysm headache, liver diseases, hypertension, cerebral aneurysm, concussion, hemodialysis, meningitis, stroke, dementia, hydrocephalus and pre-eclampsia.
 Intracranial compliance is the brain’s natural ability to stabilize intracranial pressure preventing its increase.
Intracranial compliance is the brain’s natural ability to stabilize intracranial pressure preventing its increase.
learn more about icp
what is icp?
Intracranial pressure (ICP) represents the relationship between altered skull volume and the ability of the intracranial axis system to accommodate such volume. the principles of intracranial pressure (ICP) were described by monro and kellie in the 1820s. They noted that, in adults, the brain is enclosed in a skeletal structure and that the volume present therein must remain constant so that the icp also remains constant.
The total volume inside the skull is calculated by the sum of the compartments of cerebrospinal fluid, blood and brain tissue. cerebral blood flow is constantly maintained by self-regulating mechanisms, so when a volume is added to the system or there is a pathological component, the compensatory mechanisms (e.g., the displacement of cerebrospinal fluid into the subarachnoid space of the spine and reduction of cerebral intravascular volume) operate to maintain icp constant. the current values of normality are between 3 and 22 mmhg.
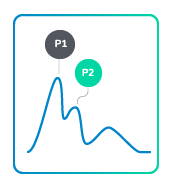
what is icp waveform?
In each cardiac cycle, the blood flow to the encephalus causes the ICP wave, which is a modified blood pressure wave. This wave has three distinct components related to the physiological parameters. the first peak (P1) is the percussion wave and reflects the blood pressure transmitted from the choroid plexus to the cerebral ventricle. The second peak (P2) is related to brain tissue complacency. It is variable and increases its amplitude as brain compliance decreases; when it exceeds the p1 wave level, it suggests an important decrease in brain compliance. Finally, the P3 wave is associated with aortic valve closure.¹
1. PEREZ-BARBACENA, J.; LLOMPART-POU, J. A.; O’PHELAN, K. H. Intracranial pressure monitoring and management of intracranial hypertension. Critical care clinics, v. 30, n. 4, p. 735-750, 1 oct. 2014.
how do we interpret the icp waveform?
Under normal icp conditions, the amplitude of these peaks is such that P1> P2> P3, which produces a characteristic wave pattern. However, when brain compliance is impaired or ICP is high, the morphology of these pulse deviates from this pattern by increasing the P2/P1 amplitude ratio.
Thus, the ICP waveform morphology, independent of absolute pressure values, is indicative of intracranial hypertension and alteration in brain compliance. This can assist in the diagnosis, treatments and lifesaving.⁸
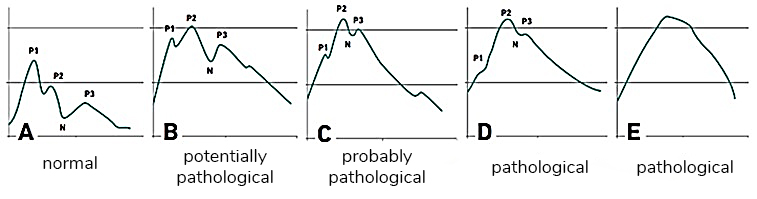
a: class i – normal; b: class ii – potentially pathological; c: class iii – probably pathological; d and e: class iv – pathological. P1 – systolic peak, P2 – current peak, n – dichrotic notch, P3 – dichrotic peak.
*Source: NUCCI, C. G. et al. (2016) Intracranial pressure wave morphological classification: automated analysis and clinical validation. Acta neurochirurgica, v. 158, n. 3, p. 581-8; discussion 588, 8.
7. DIAS, C. et al. Plateau Waves of Intracranial Pressure and Multimodal Brain Monitoring. Acta neurochirurgica. Supplement, v. 122, p. 143-146, 2014.
8. NUCCI, C. G. et al. Intracranial pressure wave morphological classification: automated analysis and clinical validation. Acta neurochirurgica, v. 158, n. 3, p. 581-8; discussion 588, 8 mar. 2016.
what are the current methods for measuring icp?
Several methods of ICP monitoring have been described, but two are frequently used in clinical practice: intraventricular and intraparenchymal catheters. ¹⁻⁹ There is a potential risk of difficulty/impossibility to position the catheter in case of ventricular compression or obstruction, from which alternative locations for intracranial monitoring were developed. additionally, the use of an intraventricular catheter can lead to infections in 5% to 10% of the cases.¹¹
1. PEREZ-BARBACENA, J .; LLOMPART-POU, JA; O’PHELAN, KH Intracranial pressure monitoring and management of intracranial hypertension. Critical Care Clinics, v. 30, n. 4, p. 735-750, 1 out. 2014.
2. COOPER, DJ et al. Decompressive craniectomy in diffuse traumatic brain injury. The New England Journal of Medicine, v. 364, n. 16, p. 1493-1502, April 21. 2011.
3. CARNEY, Nancy et al. Guidelines for the Management of Severe Traumatic Brain Injury, Fourth Edition. Neurosurgery v. 80, n. 1, p. 6-15, 1 Jan. 2017. Available in:. doi: 10.1227 / NEU.0000000000001432. Accessed on: 11 Dec. 2018.
4. MARMAROU, A. et al. Contribution of CSF and vascular factors to elevation of ICP in severely head-injured patients. Journal of neurosurgery v. 66, n. 6, p. 883-890, 1 Jun. 1987. Available at:. Accessed on: 11 Dec. 2018.
5. FAN, Jun-Yu et al. Intracranial pressure waveform morphology and intracranial adaptive capacity. American journal of critical care: an official publication, American Association of Critical Care Nurses v. 17, n. 6, p. 545-554, Nov. 1, 2008. Available at:. Accessed on: 11 Dec. 2018.
6. KASPROWICZ, Magdalena et al. Association between ICP pulse waveform morphology and ICP B waves. Neurochirurgical record. Supplement v. 114, p. 29-34, 2010. Available at:. Accessed on: 11 Dec. 2018.
7. DIAS, C. et al. Plateau Waves of Intracranial Pressure and Multimodal Brain Monitoring. Neurochirurgical record. Supplement, v. 122, p. 143-146, 2014.
8. NUCCI, CG et al. Intracranial pressure wave morphological classification: automated analysis and clinical validation. Acta neurochirurgica, v. 158, n. 3, p. 581-8; discussion 588, 8 Mar. 2016.
9. MARSHALL, Scott A et al. Management of intracerebral pressure in the neurosciences critical care unit. Neurosurgery clinics of North America v. 24, n. 3, p. 361-373, 24 Jul. 2013. Available in:. Accessed on: 11 Dec. 2018.
11. LOZIER, Alan P et al. Ventriculostomy-related infections: a critical review of the literature. Neurosurgery v. 51, n. 1, p. 170-81; discussion 181, 1 jul. 2002. Available at:. Accessed on: 11 Dec. 2018.
are there other non-invasive ways to monitor icp?
Because of its relevance, several initiatives for the noninvasive evaluation of ICP have been developed in the world over the last 50 years, with varying degrees of diagnostic accuracy when compared to invasive methods: doppler transcranial ultrasonography (dtc)¹⁴, skull vibrations¹⁵, brain tissue resonance¹⁶, transcranial time-of-flight¹⁷, venous ophthalmodynamometry¹⁸, assessment of the optic nerve sheath diameter (onsd)¹⁹, displacement of the tympanic membrane²⁰⁻²¹, otoacoustic emissions²², magnetic resonance imaging (mri) to estimate intracranial compliance²³, guided eyeball compression by ultrasound²⁴ and recording of visual evoked potentials²⁵. These different initiatives attempt to overcome the challenges of providing the icp pulse waveform , the absolute value in mmhg, the continuous monitoring capability and the icp trend over time.
14. HANLO, PW et al. Monitoring intracranial dynamics by transcranial Doppler-a new Doppler index: trans systolic time. Ultrasound in medicine & biology, v. 21, n. 5, p. 613-621, 1993.
15. Ueno, T. et al. Noninvasive measurement of pulsatile intracranial pressure using ultrasound. Neurochirurgical record. Supplement, v. 71, p. 66-69, 1996.
16. MICHAELI, D.; RAPPAPORT, ZH Tissue resonance analysis; a novel method for noninvasive monitoring of intracranial pressure. Technical note. Journal of neurosurgery, v. 96, n. 6, p. 1132-1137, 1 Jun. 2002.
17. RAGAUSKAS, A. et al. Implementation of non-invasive brain physiological monitoring concepts. Medical engineering & physics, v. 25, n. 8, p. 667-678, 1 out. 2003.
18. QUERFURTH, HW et al. Ophthalmodynamometry for ICP prediction and pilot test on Mt. Everest. BMC neurology, v. 10, p. 106, 1 Nov. 2010.
19. GEERAERTS, T. et al. Ultrasonography of the optic nerve sheath may be useful for detecting raised intracranial pressure after severe brain injury. Intensive care medicine, v. 33, n. 10, p. 1704-1711, 1 out. 2007.
20. REID, A. et al. Mean intracranial pressure monitoring by a non-invasive audiological technique: a pilot study. Journal of Neurology, Neurosurgery, and Psychiatry, v. 52, n. 5, p. 610-612, May 1, 1989.
21. SHIMBLES, S. et al. Clinical comparison of tympanic membrane displacement with invasive intracranial pressure measurements. Physiological measurement, v. 26, n. 6, p. 1085-1092, Dec. 7, 2005.
22. FRANK, AM et al. Non-invasive measurement of intracranial pressure changes by otoacoustic emissions (OAEs) -a report of preliminary data. Zentralblatt fur Neurochirurgie, v. 61, n. 4, p. 177-180, 1998.
23. ALPERIN, NJ et al. MR-Intracranial pressure (ICP): a method to measure intracranial elastance and pressure noninvasively by means of MR imaging: baboon and human study. Radiology, v. 217, n. 3, p. 877-885, 1 dez. 2000.
24. BARTUSIS L, et al. Ophthalmic artery as a non-invasive intracranial pressure measurement electronic system. Elektron ir Elektrotechnika. 2012; 122 (6): 45-8.
25. ZHAO, YL; ZHOU, JY; ZHU, GH Clinical experience with the noninvasive ICP monitoring system. Neurochirurgical record. Supplement, v. 95, p. 351-355, 2003.
what is the principle of operation for brain4care noninvasive method
The principle of operation for the non-invasive monitoring of icp waveform is based on the study conclusions of professor sérgio mascarenhas, that detected changes in icp waveform through small variations in the volume of the skull and the commonly accepted principles of icp waveform morphology.
The device (sensor) consists of tension gauges attached to a cantilever bar that is supported on a headband placed on the patient’s head. The sensor is positioned perpendicularly at the temporoparietal transition, 2 inches (5-6cm) above the entrance of the external auditory canal in the coronal plane, and a slight pressure is applied to ensure that the sensor stays in contact with the scalp.
When blood is pumped into the brain, the skull undergoes small deformations due to pressure variations, and these local deformations lead to the expansion and compression of the skull against that headband and sensor. The headband, besides positioning the sensor on the correct place, also transmits the forces of skull expansion and contraction that go against it to the sensor pin resulting in the pin movement that is then translated to a variation in sensor voltage.
The device continuously transmits the sensor voltage signal and sends it to a multiparameter monitoring device that digitizes, filters and amplifies the received signal and displays the surrogate ICP waveform morphology of the corresponding waveform and its trend over time.
how many peaks can be identified in the curve?
The medical team evaluates the amplitude and characteristic of waveform peaks P1, P2, P3 displayed to assess the patient’s clinical status.
what is cpp?
Cerebral perfusion pressure (cpp) is the pressure gradient that allows blood flow to the intracranial constituents. cpp is equal to mean arterial pressure (map) minus venous pressure (vp). In humans, pressure in the venous sinuses is difficult to measure, and because vp occurs in parallel to icp, cpp is considered to be equal to the difference between map and ICP.²⁶
26. CARLOTTI JR., C. ; COLLI, B .; DIAS, L. Intracranial hypertension. Medicine (Ribeirão Preto, Online), v. 31, n. 4, p. 552-562, Dec. 30th. 1998
what is cbf?
Cerebral blood flow (cbf) is the amount of blood supplied to the brain at any given time, and is related to brain activity. cbf and cpp are directly proportional.²⁶
26. CARLOTTI JR., C. ; COLLI, B .; DIAS, L. Intracranial hypertension. Medicine (Ribeirão Preto, Online), v. 31, n. 4, p. 552-562, Dec. 30th. 1998
what is the monro-kellie doctrine?
The principles of intracranial pressure (ICP) were described by monro and kellie in the 1820s. They noted that, in adults, the brain is enclosed in a skeletal structure and that the volume present therein must remain constant so that the ICP also remains constant. ¹
According to the monro-kellie doctrine, the skull cannot be expanded after the closing of the fontanelles and this doctrine has been accepted and followed for the last two centuries.
26. PEREZ-BARBACENA, J.; LLOMPART-POU, J. A.; O’PHELAN, K. H. Intracranial pressure monitoring and management of intracranial hypertension. Critical care clinics, v. 30, n. 4, p. 735-750, 1 oct. 2014.
what are the main symptoms of intracranial hypertension?
Symptoms of intracranial hypertension include:
- headache;
- alterations on vision;
- nausea;
- vomiting;
- dizziness;
- somnolence;
- spontaneous release.
what are the main pathological causes of intracranial hypertension?
Intracranial hypertension (ich) is a common and clinically important event in patients with severe traumatic brain injury (tbi), ischemic stroke (ischemic stroke) long, subarachnoid hemorrhage (sah) and intracerebral hemorrhage (hip)²⁸ the ich can be the final event of several intracranial catastrophes. This is because the increase in icp invariably triggers a fall in cpp, blood flow and, as a consequence, we have focal and/or global ischemia.
28. JORDAN, KG Neurophysiologic monitoring in the neuroscience intensive care unit. Neurologic clinics, v. 13, n. 3, p. 579-626, 1 Aug. 1995.
what is the relation between blood pressure and icp?
ICP waveform morphology is dependent on the blood pressure waveform due to the interaction between blood pressure and intracranial components, I.e. brain tissue, csf, and arterial and venous blood.³⁰
The normal encephalus has self-regulation capacity for cerebral blood flow (cbf) ensuring a constant blood flow to the brain through cerebral vessels. In normal conditions, the cerebral circulation adapts to the arterial pressure variations to maintain the cbf constant. In this way, an increase in blood pressure (bp) is prevented from increasing cbf and consequently icp, and also a decrease in blood pressure (bp) is prevented from reducing cerebral vascular resistance (cvr), in order to maintain cbf. this maintains cerebral perfusion pressure (cpp) adequate for the efficient function of brain activities.³¹
30. TAKIZAWA, H .; GABRA-SANDERS, T .; MILLER, JD Changes in the cerebrospinal fluid pulse wave spectrum associated with raised intracranial pressure. Neurosurgery v. 20, n. 3, p. 355-361, 1 March. 1987. Available at:. Accessed on: Dec. 13 2018.
31. GUASTELLI, LR; RIBAS, MR; ROSA, CACA Intracranial pressure. In: KNOBEL, E. Intensive Care Nursing. São Paulo: Editora Atheneu, 2006. p. 321-331.
can the absolute number of the icp be within normal threshold while the patient suffers a loss in intracranial compliance? if so, how can one identify it?
Yes.
The change in mean values of ICP is usually monitored in neurosurgical units, although it is a “late” event in the pathophysiological cascade³² and is not always present in pathological conditions, such as in normal pressure hydrocephaly.
Therefore, the waveform of the icp morphology, independent of the absolute pressure values, is indicative of intracranial hypertension and altered cerebral complacency.⁸
32 MORGALLA, M. H; STUMM, F .; HESSE, G. A computer-based method for continuous single pulse analysis of intracranial pressure waves. Journal of the Neurological Sciences v. 168, n. 2, p. 90-95, Oct. 15. 1999. Available at:. Accessed on: Dec. 13 2018.
8. NUCCI, CG et al. Intracranial pressure wave morphological classification: automated analysis and clinical validation. Acta neurochirurgica, v. 158, n. 3, p. 581-8; discussion 588, 8 Mar. 2016